So here it is, my very LONG, open and honest blog post about my 104 interesting days on Escitalopram (aka Lexapro/Cipralex)
💊 💊 💊
Timeline
- 7th February – 10mg
- 23rd February – 20mg
- 16th March – 10mg
- 20th April – First appointment with Psychologist
- 11th May – 5mg
- 21st May – Last 5mg pill
Mental health is still a topic that is often kept in the dark. Even myself is guilty of this. In the past, I have been diagnosed with both depression and anxiety. I have had counselling, and have also taken alternative antidepressants such as 5-HTP and St. Johns Wort – all of which was without the knowledge of my family and friends.
The genetic result that I received in November, ignited my anxiety. Over the Christmas period, I experienced episodes of high blood pressure and on some occasions, panic attacks. These would go on for 30 minutes or so as they continuously flared back up, thus resulting in me taking Valium to calm myself down.
Over the years, I’ve done my own research into antidepressants and their side-effects and was strongly against taking them myself. But in February, after experiencing more panic attacks relating to my ongoing health issue (I also took 5-HTP during this period and it wasn’t helping), I went to my Doctor and asked for antidepressants, because I felt that I couldn’t manage this on my own. At the same time, I was also referred to a Clinical Psychologist.
7th February – Diary Extract (10mg) How it affected my emotions
Today I went to the doctors and took my first antidepressant. After struggling (but managing) for over 10 years, I finally caved. The anxiety has gotten the better of me, thus in turn making my depression bad. At the moment, I’m a mess. This new revelation of me having this crappy gene mutation, has been a tough pill to swallow. I thought I was coping well, but as usual, I was downplaying it and fooling myself. Last week was hell. I barely left the house. Hell, I barely even got dressed or left the bed. That’s when I really knew I had to seek help and sort it out because I wasn’t able to sort it myself. I’m feeling a lot of mixed emotions. I’m nervous and anxious to be taking this medication, as it’s something I wanted to avoid. I’m sad because I feel defeated, that I could no longer help or control myself mentally… But I also feel proud, for making the appointment, going there and explaining myself so well that I got the outcome that I had hoped for.
At 00:30, I came home and wrote in my diary after being out with a group of people. I didn’t drink alcohol as I wasn’t sure how it would affect me. But I left early as I was feeling very uncomfortable in this social situation.
I feel that the medication has affected me already. Today I felt mellow, but not like I do with Valium, just calm and level with a bit of a fuzzy head… Tonight, I left early since I could feel my anxiety bubbling to the surface. As I walked home, I wanted to cry, but I couldn’t. Here I am feeling sad – but level, with no tears.
21st February – Diary Extract (10mg) Feeling mentally drained and demotivated
Today I feel rubbish. My 13th day on Lexapro and my head is a mess. No motivation. No real desire to eat. I feel hungry – but I feel like I’ve lost all motivation completely. It’s been difficult to go to the gym as my head has felt cloudy and my focus has been off. I’m so tired all the time, I just want to rest. I’m tired, but I can’t nap and it’s mentally draining. I don’t have an appointment yet to see a Psychologist – I almost can’t be bothered going to see one anymore. My health anxiety has subsided for now, but today I feel as though it (Lexapro) may not be worth it. I know I need to stick it out for a few more weeks at least.
23rd February
I had a follow up appointment with my Doctor and mentioned that it had curbed my health anxiety. I also spoke about the crippling exhaustion and tiredness that I had been experiencing, along with my lack of motivation to do anything. The Doctor did not believe that this was related to the medication, and advised me to increase the dosage to 20mg.
19th April – Diary Extract
So a lot has happened since I last wrote in here. The side-effects were awful at 20mg. I was spaced out like a zombie, had no energy whatsoever and couldn’t focus or do anything at the gym. So after two weeks, I tapered back down to 10mg. I still have tiresome days.
During my time on 20mg, my behaviour was strange. B would find me sitting and staring into space. When I did this, I wasn’t day-dreaming – I was simply staring into the abyss. Looking back at this time, I said “the lights were on but nobody was home”. This is not something I would ever want to experience again…
During my sessions with a Psychologist, I mentioned the tiredness, exhaustion and inability to do the things that I once enjoyed – eg, go to the gym, cook, hang out with friends… I also made it clear that I wanted to stop taking the antidepressants because I felt that they were suppressing my emotions. I hadn’t cried properly in months and I just felt constantly flat. The Psychologist explained that the anxiety, depression and sadness that I had been experiencing prior to me taking the medication was a natural human response to something real that I was going through. It made a lot of sense. I wasn’t feeling depressed for no reason, and the panic attacks weren’t random either. I was genuinely upset and scared of what I had recently found out, and hadn’t had enough time to process it all.
I wad advised not to quit taking the tablets cold-turkey, so on the 11th May, I began cutting my pills in half and took 5mg daily. Slowly but surely, I felt that I had a bit more energy and was returning to my normal self .
On the 21st May, I took my last 5mg dose of Lexapro.
I mentioned at the start of this post that I was well aware of the side-effects of antidepressants (not so much the tiredness part though – I should have NEVER increased my dosage to 20mg), but I was not well-informed or clued up about the withdrawals. A lot of that, was naivety on my part since 5-HTP and St. Johns Wort never gave me any. A quick google search led me to many posts on forums about “brain zaps” and “brain shivers”, and how many people resorted back to antidepressants because of the withdrawals.
The first week was awful. I felt generally dizzy (as though I had lost my sense of balance) and my brain felt fuzzy. Whenever I moved my head from side to side, I would feel a strange zappy feeling in my brain. Sometimes, the shock sensation would radiate down my arm. Despite this, I persevered. I took a 100mg dose of 5-HTP twice a day, and magnesium before bed in hope that this would help.
I’m almost 2 weeks “clean” and can honestly say, never again. I still get the strange zappy feelings now and then, but they’re nowhere near as intense as they initially were. My emotions have returned (I actually cried the other day, and it felt so good to let it all out!) and my motivation is back! Once again, I enjoy going to the gym and cooking. 🙂
Perhaps all I needed was time. Maybe the antidepressants were good for short-term use in my case, whilst I got my head around all of this.
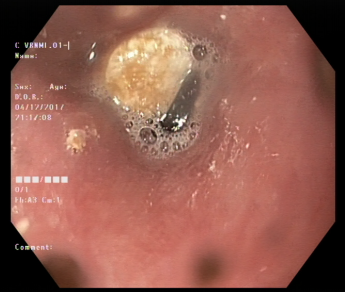
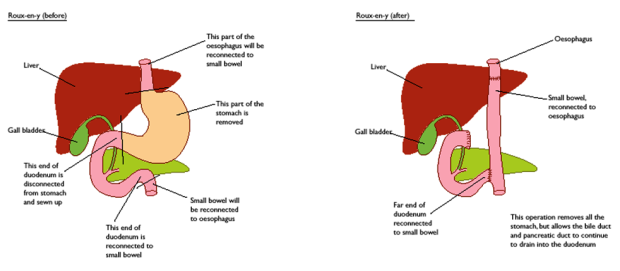
Right now I feel positive, even though I’m having my stomach removed in a few months time since one of my biopsies showed cancer (and this is me talking without the Lexapro in my system!) My plan is to make the most out of the next few months,make lots of plans, enjoy myself and eat/drink whatever I want, whenever I want! ❤
Disclaimer: As the author of this blog, I have based my writings upon my own experiences regarding the topics covered in my post. However, I am not a medical doctor, nurse or otherwise formally qualified in this subject matter. The information contained in this blog is not intended to be construed in any manner as medical advice.




































 Looking back, I’m just glad that I didn’t take the paracetamol tablets that were offered to me the day after surgery! I told them that this would be too difficult for me to swallow, so they gave me it intravenously instead. I even asked for a prescription of dissolvable paracetamol when I was discharged from hospital, as the regular tablets are so large and round in Norway!
Looking back, I’m just glad that I didn’t take the paracetamol tablets that were offered to me the day after surgery! I told them that this would be too difficult for me to swallow, so they gave me it intravenously instead. I even asked for a prescription of dissolvable paracetamol when I was discharged from hospital, as the regular tablets are so large and round in Norway!














 Today has been a much better day! The pain has been managed throughout the night, which meant I got a lot of sleep and some during the day too. I also drank 1.5 cups of tea, 1 cup of lemon water and a bit of saft. So I feel like I’ve managed to get a lot down today. It’s also been nice having more visitors as Linda came to spend the afternoon with me. She brought me a lovely pink lotus flower friendship bracelet, that she also has in blue. Very thoughtful ❤ B also came to visit later in the day and he’s just getting ready to leave. Later, I’ll give my mum a call and maybe try to read my book. It’s so difficult though as my eyes keep rolling around in the back of my head as I feel tired all of the time.
Today has been a much better day! The pain has been managed throughout the night, which meant I got a lot of sleep and some during the day too. I also drank 1.5 cups of tea, 1 cup of lemon water and a bit of saft. So I feel like I’ve managed to get a lot down today. It’s also been nice having more visitors as Linda came to spend the afternoon with me. She brought me a lovely pink lotus flower friendship bracelet, that she also has in blue. Very thoughtful ❤ B also came to visit later in the day and he’s just getting ready to leave. Later, I’ll give my mum a call and maybe try to read my book. It’s so difficult though as my eyes keep rolling around in the back of my head as I feel tired all of the time.

 Today they removed my drain! At first, the nurse removed the bandage, and then the stitches. She gave me morphine and suggested I walked around for 10 minutes to loosen the drain. I’m squeamish with needles and stuff like that, so it grossed me out to look down and see a tube sticking out of my abdomen! It was a bit painful as I was walking around and I started to get dizzy just before she came back into the room. It was painful when she pulled it out! I yelled out that loud, I’m sure the whole ward could hear me! I still have a lot of discomfort in the area, but it’s no surprise really as it was through my muscle.
Today they removed my drain! At first, the nurse removed the bandage, and then the stitches. She gave me morphine and suggested I walked around for 10 minutes to loosen the drain. I’m squeamish with needles and stuff like that, so it grossed me out to look down and see a tube sticking out of my abdomen! It was a bit painful as I was walking around and I started to get dizzy just before she came back into the room. It was painful when she pulled it out! I yelled out that loud, I’m sure the whole ward could hear me! I still have a lot of discomfort in the area, but it’s no surprise really as it was through my muscle. Today I’m going home! They said I could stay another night if I didn’t feel safe leaving today, but I feel ready. I still have some discomfort, but I’m coping well without morphine.
Today I’m going home! They said I could stay another night if I didn’t feel safe leaving today, but I feel ready. I still have some discomfort, but I’m coping well without morphine.