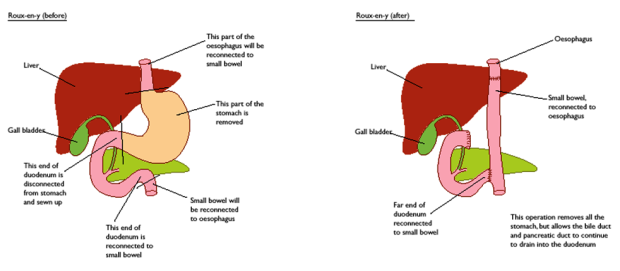
On the 26th September, I kissed goodbye to my stomach. Why? Well, to cut a long story short, I inherited a mutation in the CDH1 gene – which means I have an increased chance of developing diffuse gastric cancer and lobular breast cancer. After a routine gastroscopy in April revealed one of the biopsies to show cancer, I made the decision to have a total gastrectomy. Below are extracts from my diary that I wrote during my stay in hospital.

Stomach Plush – Bought from Plusheez
26.09.17 Day of Surgery – Tuesday
Today is the day. Something I’ve been building towards for the past 4 months, ever since I got that phone call on the 18th May. Currently sitting in hospital in pjs and a dressing gown, trying to keep as cosy and warm as possible. B is sitting here beside me, usually sleeping as he’s shattered. We were here 8.5 hours yesterday for my pre-op so we were both exhausted! Luckily they gave me a sleeping pill to knock me out last night. Starting to get a bit nervous now. Just trying not to think about it all as I keep visualising myself in the operating room and it freaks me out a bit. It’s a long road ahead, but I have to do this. The alternative would or could be much worse…
27.09.17 Day 1 – Wednesday

So yesterday went well. The level of care here has been fantastic so far. The surgery took longer than the expected 3-4 hours. I was under anaesthesia for 9 hours! This is because they sent some tissue to pathology for testing to see if there was any gastric mucosa left behind where they made the join of the oesophagus to the small intestine. It turned out that there was, so they cut more tissue away and made a new join. When the surgeons told me this today, I thanked them massively as having stomach mucosa left behind had been my biggest worry. They allowed B to come and see me in the recovery ward at around 10pm last night. They said I would be incoherent and wouldn’t remember anything, but I was fine! Even the nurses were shocked! When they awoke me from surgery, I even asked them what time it was and was surprised at realising that I had been asleep for 9 hours!
Today I am allowed to drink 300ml of water, but it’s a struggle. When I take a sip, it feels like it gets trapped in my throat and chest, so I sucked on ice cubes instead. Unfortunately, that’s now causing the same issue. I managed to get up onto my feet with the help of the nurses, so that’s something at least! Baby steps – one day at a time. I will try again tomorrow. Apparently I look well and have no fever, so that’s a good start.
28.09.17 Day 2 – Thursday

So today, the physiotherapist got me up and walking down the corridor and back! My main struggle is the air that’s trapped in my body. A lot of it is in my chest and some further down. The pain is horrific! Turns out it’s from the CO2 that was pumped into me during surgery. They said most of it will be absorbed by the body and muscles over the next few days. B came to visit again today, it’s really great having him here. I haven’t done much at all today apart from rest but surprisingly, it hasn’t been boring. I just need to remember that my body needs time for everything to heal, so rest is very important. I also managed to drink half a glass of saft! Small victories!
29.09.17 Day 3 – Friday

Sitting Upright

Walking

Flowers from Gianni
Last night wasn’t so good. I think I called for the nurse 3 times because of the pain caused by the trapped CO2. Today was okay, I walked three times with the IV stand (no longer need the zimmer frame thing!) and I can even walk without it whilst someone else pushes it along for me! The only downside is that it’s pushing around all the air inside me when I walk. I’ve cried twice today from the pain because it’s so bad and now it’s pushing against my incision where my stitches are. If I didn’t have to deal with this, I feel it would be plainer sailing! Gianni stopped by today with Bjørnar, and brought me a beautiful potted plant. It was nice having extra visitors. It was also nice being able to catch up with him, as I havn’t seen him for a couple of months. B has been wonderful though, attending to some nurse type things whilst I’m in here, what a saint.
30.09.17 Day 4 – Saturday

My Room

Flowers from BK & Anne Marthe
Last night also wasn’t good. I called for the nurse 4 times because of the pain caused by the air. Each time, they increased my epidural and I would fall asleep only to wake again an hour later in agony. On the fourth call, they gave me morphine and I slept for 3 hours until the nurses came in at 7am.
Today has been a struggle. My epidural was removed, as well as my catheter. The pain has been the same as last night. Over the course of the day, they managed to get the pain under control by giving me morphine. BK and Anne Marthe came to visit in the afternoon, which was lovely 🙂 They brought me a beautiful bouquet of purple flowers. Weirdly enough I felt a bit guilty because I was very drugged up and still in a lot of pain, so I wasn’t much fun to be around!
01.10.17 Day 5 – Sunday
 Today has been a much better day! The pain has been managed throughout the night, which meant I got a lot of sleep and some during the day too. I also drank 1.5 cups of tea, 1 cup of lemon water and a bit of saft. So I feel like I’ve managed to get a lot down today. It’s also been nice having more visitors as Linda came to spend the afternoon with me. She brought me a lovely pink lotus flower friendship bracelet, that she also has in blue. Very thoughtful ❤ B also came to visit later in the day and he’s just getting ready to leave. Later, I’ll give my mum a call and maybe try to read my book. It’s so difficult though as my eyes keep rolling around in the back of my head as I feel tired all of the time.
Today has been a much better day! The pain has been managed throughout the night, which meant I got a lot of sleep and some during the day too. I also drank 1.5 cups of tea, 1 cup of lemon water and a bit of saft. So I feel like I’ve managed to get a lot down today. It’s also been nice having more visitors as Linda came to spend the afternoon with me. She brought me a lovely pink lotus flower friendship bracelet, that she also has in blue. Very thoughtful ❤ B also came to visit later in the day and he’s just getting ready to leave. Later, I’ll give my mum a call and maybe try to read my book. It’s so difficult though as my eyes keep rolling around in the back of my head as I feel tired all of the time.
02.10.17 Day 6 – Monday

Me and Vigdis

Flowers from Vigdis
Today has been an interesting one. I was sent for a chest x-ray at 9pm last night. (I’ve been wheezing a little bit when I breathe in and out.) Turns out, I have a bit of fluid on my lungs. No infection though, so I have to be mindful to take deep breaths and be up and about more. B and his mum came to visit me in the afternoon. It was lovely having her here as I didn’t know she was going to be in town until I was in hospital. She brought me a beautiful bowl of flowers, which one of the nurses commented on saying how pretty it was.
Today I’ve started to eat a few things. I say eat, but it’s still liquids. First off, I tried a chicken stock cube in hot water (too salty as I used the whole cube in a small amount of water – silly me), then i had 3/4 of a high calorie berry protein shake and a bit of fiskesuppe. My appetite seems to have changed though. I absolutely loved fiskesuppe before, but once it was in front of me, the smell made me feel nauseous. I tried a couple of spoonfuls and couldn’t have any more. Today I’ve been walking up and down the stairwell! Managed to do it three times as they suggested. At the moment, I have a lot of strength as I’m given saline and glucose via IV. Tomorrow they’re planning on removing my drainage tube. That’s the source of a lot of my pain, so hopefully once that’s out, things will get a little easier.
03.10.17 Day 7 – Tuesday
 Today they removed my drain! At first, the nurse removed the bandage, and then the stitches. She gave me morphine and suggested I walked around for 10 minutes to loosen the drain. I’m squeamish with needles and stuff like that, so it grossed me out to look down and see a tube sticking out of my abdomen! It was a bit painful as I was walking around and I started to get dizzy just before she came back into the room. It was painful when she pulled it out! I yelled out that loud, I’m sure the whole ward could hear me! I still have a lot of discomfort in the area, but it’s no surprise really as it was through my muscle.
Today they removed my drain! At first, the nurse removed the bandage, and then the stitches. She gave me morphine and suggested I walked around for 10 minutes to loosen the drain. I’m squeamish with needles and stuff like that, so it grossed me out to look down and see a tube sticking out of my abdomen! It was a bit painful as I was walking around and I started to get dizzy just before she came back into the room. It was painful when she pulled it out! I yelled out that loud, I’m sure the whole ward could hear me! I still have a lot of discomfort in the area, but it’s no surprise really as it was through my muscle.
It’s now 9:30pm and someone has been wheeled into my room 😦 Boo! I had it so good! I was initially sharing a room with somebody until Friday, so it was nice having a space to myself for a few days. Never mind, I should only be here for another few nights.
04.10.17 Day 8 – Wednesday
 Today I’m going home! They said I could stay another night if I didn’t feel safe leaving today, but I feel ready. I still have some discomfort, but I’m coping well without morphine.
Today I’m going home! They said I could stay another night if I didn’t feel safe leaving today, but I feel ready. I still have some discomfort, but I’m coping well without morphine.
I’m still trying to eat as often as possible. I got a bit dizzy in the pharmacy earlier, and figured it was my blood sugar level. So I had a teeny bit of honey once I got home, which seemed to help. I even tried a mashed up poached egg in the evening! It’s nice to be home and trying different foods and being back with B ❤
I just want to say a huge thank you to the wonderful Nurses, Doctors and Surgeons at Haukeland that looked after me during my stay, thanks for the lovely messages of support and kind words from my family and friends, thanks to my wonderful visitors that came to see me in hospital, which made my time spent there much more pleasant… and the biggest thank you of all to Nurse B ❤
Not sure how I could have gone through this without him.






































 Today has been a much better day! The pain has been managed throughout the night, which meant I got a lot of sleep and some during the day too. I also drank 1.5 cups of tea, 1 cup of lemon water and a bit of saft. So I feel like I’ve managed to get a lot down today. It’s also been nice having more visitors as Linda came to spend the afternoon with me. She brought me a lovely pink lotus flower friendship bracelet, that she also has in blue. Very thoughtful ❤ B also came to visit later in the day and he’s just getting ready to leave. Later, I’ll give my mum a call and maybe try to read my book. It’s so difficult though as my eyes keep rolling around in the back of my head as I feel tired all of the time.
Today has been a much better day! The pain has been managed throughout the night, which meant I got a lot of sleep and some during the day too. I also drank 1.5 cups of tea, 1 cup of lemon water and a bit of saft. So I feel like I’ve managed to get a lot down today. It’s also been nice having more visitors as Linda came to spend the afternoon with me. She brought me a lovely pink lotus flower friendship bracelet, that she also has in blue. Very thoughtful ❤ B also came to visit later in the day and he’s just getting ready to leave. Later, I’ll give my mum a call and maybe try to read my book. It’s so difficult though as my eyes keep rolling around in the back of my head as I feel tired all of the time.

 Today they removed my drain! At first, the nurse removed the bandage, and then the stitches. She gave me morphine and suggested I walked around for 10 minutes to loosen the drain. I’m squeamish with needles and stuff like that, so it grossed me out to look down and see a tube sticking out of my abdomen! It was a bit painful as I was walking around and I started to get dizzy just before she came back into the room. It was painful when she pulled it out! I yelled out that loud, I’m sure the whole ward could hear me! I still have a lot of discomfort in the area, but it’s no surprise really as it was through my muscle.
Today they removed my drain! At first, the nurse removed the bandage, and then the stitches. She gave me morphine and suggested I walked around for 10 minutes to loosen the drain. I’m squeamish with needles and stuff like that, so it grossed me out to look down and see a tube sticking out of my abdomen! It was a bit painful as I was walking around and I started to get dizzy just before she came back into the room. It was painful when she pulled it out! I yelled out that loud, I’m sure the whole ward could hear me! I still have a lot of discomfort in the area, but it’s no surprise really as it was through my muscle. Today I’m going home! They said I could stay another night if I didn’t feel safe leaving today, but I feel ready. I still have some discomfort, but I’m coping well without morphine.
Today I’m going home! They said I could stay another night if I didn’t feel safe leaving today, but I feel ready. I still have some discomfort, but I’m coping well without morphine.